Home / Degrees / Healthcare / MSN / Master of Science in Nursing - Family Nurse Practitioner / Explore MSN FNP
Questions to Consider: The MSN Family Nurse Practitioner Degree

If you’re ready to take your nursing practice to the next level, becoming a family nurse practitioner (FNP) might be the right choice for you. By providing preventive treatment and disease management to diverse populations, board-certified FNPs are a valuable resource. Advanced clinicians, such as those who graduate from the online Master of Science in Nursing (MSN) – FNP program at St. Thomas University (STU), play an active and mostly independent role in patient care.
FNPs enjoy almost as many privileges and responsibilities as medical doctors, and they’re filling the gap in primary care. Amid a growing shortage of generalist physicians, the role of nurse practitioner is one of the fastest-growing occupations in healthcare. In fact, it’s one of the fastest-growing occupations across all industries in the U.S.
An MSN is the first step to FNP certification. With an online MSN – Family Nurse Practitioner program, you’ll maintain your current employment, customize your schedule and complete clinical hours at a site of your choosing. Follow the links below to learn about specific elements of the program.
What Is an MSN FNP Degree?

The online MSN – FNP program at STU is a CCNE-accredited graduate degree that prepares RNs for advanced practice roles in family healthcare. It puts you on track to become a board-certified family nurse practitioner. To accomplish this, the degree provides advanced knowledge in health promotion, illness prevention, diagnosis and disease management.
You’ll develop strategies for treating individuals, families and communities as you move through the degree program. Standard courses center on knowledge acquisition through reading, writing, research and discussion. Clinical courses offer hands-on experience. You’ll hone your skills as a primary care provider through this two-pronged approach to learning.
Online programs, like the MSN – FNP at St. Thomas University, are designed for working nurses. Even nurses with split shifts and on-call schedules can take advantage of the online format. That’s because courses are accessible 24/7.
How Do You Become a Nurse Practitioner?
After you’ve earned a bachelor’s degree in nursing and passed the NCLEX-RN exam, you’ll want to gain a couple of years of experience as a registered nurse before taking the next step, which is to earn a graduate degree.
A master’s or doctoral degree is required to become a nurse practitioner in the U.S., according to the American Association of Nurse Practitioners (AANP). After completing an MSN program or similar program, nurses then take the national board certification exam and apply for state NP licensure.
A significant majority of nurse practitioners provide primary care services, and almost 70% are certified as family nurse practitioners, the largest specialty within the NP profession. According to the AANP, 69.7% of all NPs identify as family nurse practitioners as of 2025. This specialization enables NPs to deliver comprehensive primary care to patients across all age groups and is the main driver meeting the nation’s increasing demand for primary care providers.
Of all nurse practitioners have a graduate degree
– American Association of Nurse Practitioners
Why Should You Become a Family Nurse Practitioner?

Aside from expanding your knowledge and advancing your practice (or opening your own private practice), becoming an FNP offers greater professional autonomy, and it allows you to make a significant impact on patient outcomes. You’ll gain experience working with a range of patients and health conditions, establish a foundation for preventive care and oversee the diagnosis and treatment of chronic and acute disease.
You’ll also enjoy rapid job growth as an FNP. For example, the U.S. Bureau of Labor Statistics (BLS) projects a 40% rise in employment between 2023 and 2033. FNPs benefit from low unemployment rates and rising salaries as well. According to the Advanced Practice Education Associates (APEA), salaries for FNPs went up 16% since 2018 and more than 13% for primary care NPs from 2020 to 2023.
What Does the STU Online MSN FNP Program Teach?
Online or on campus, MSN – FNP programs cover advanced clinical and diagnostic skills in primary care medicine. Courses emphasize evidence-based practice, advanced assessment and clinical decision-making skills essential for primary care delivery. Graduates of this program build and refine the following competencies to provide high-quality and culturally appropriate care across various settings and populations:
- Incorporate evidence-based research into preventive, chronic and acute care
- Advocate for policies that improve care systems and health outcomes
- Apply nursing informatics to enhance and streamline patient care
- Coordinate care delivery across interprofessional teams
- Integrate clinical treatment with health promotion strategies
Ultimately, you’ll learn everything you need to pass your board certification exam and begin your new role as a successful FNP.
Which Courses Will You Take?
MSN – FNP programs expand on your current knowledge in health assessment, pharmacology and pathophysiology. Core courses also build your expertise in evidence-based research, healthcare policy and disease prevention. From there, many FNPs-in-training will complete specialization courses across the spectrum of primary care. Clinical hours are either built into your courses or completed separately. It varies by program.
At STU, specialization courses are split into didactic and clinical modes. Each mode runs simultaneously over a period of seven weeks (or six weeks during summer terms), allowing you to implement your newfound knowledge with hands-on practice. Paired classes are conveniently arranged by patient population:
- Children and families
- Women’s health
- Adults
- Adult gerontology
Next, students at STU address health promotion, disease prevention and clinical management through the practicum course, Advanced Practice Nursing Integration.
What Are the Requirements for Admission to an MSN FNP Program?

While admission policies are set by each university and program, there are several common themes. First, you’ll need a valid, unencumbered RN license and a BSN from an accredited nursing school. Your cumulative GPA will have to meet minimum requirements as well. After that, some MSN – FNP programs may request one or more of the following:
- Letters of recommendation
- GRE scores
- Personal statement
- One to two years of clinical experience
STU’s requirements for admission are simple. Aside from your Florida or Georgia nursing license and a BSN from an accredited program, all you need is a cumulative 3.0 GPA. The program is open to all RNs living and working in Florida and Georgia.
Is Institutional Accreditation Important?
Yes, it’s very important. Institutional accreditation ensures that your university is ethically and fiscally responsible. It also guarantees positive academic outcomes and consistent graduation rates. University accreditation is required for federal financial aid, scholarships, tuition reimbursement, military education benefits and loan forgiveness programs. Because most universities won’t recognize unaccredited degrees, your opportunities for continuing education are also limited.
STU is accredited by the Southern Association of Colleges and Schools Commission on Colleges (SACSCOC). You can confirm university and program status through the U.S. Department of Education’s searchable Database of Accredited Postsecondary Institutions and Programs (DAPIP).
What’s the Difference Between Institutional Accreditation and Programmatic Accreditation?
While institutional accreditation confirms the quality of your university, programmatic accreditation guarantees the quality of your degree program. For nurses, your program should be accredited by the Commission on Collegiate Nursing Education (CCNE) or the Accreditation Commission for Education in Nursing (ACEN). CCNE- and ACEN-approved programs meet professional and industry standards.
The MSN – FNP program at St. Thomas University is CCNE-accredited. Graduates are prepared for professional certification.
How Are FNPs Certified?

There are two certification options for FNP licensing, and accredited programs should prepare you for both. The American Academy of Nurse Practitioners (AANP) and American Nurses Credentialing Center (ANCC) offer slightly different exams. Outlines and study guides are widely available, so you can select the format that works best for you.
AANP and ANCC certifications are nationally recognized, so it doesn’t really matter which exam you choose. Once you pass, you can practice as a licensed FNP throughout the U.S.
How Many Clinical Rotations Will You Complete for Your FNP Degree?

Students in STU’s MSN – FNP online program must complete 500 clinical hours. Your time is divided equally between seven-week rotations in child and family care, women’s health, adult health and gerontology.
Beyond that, your rotations are largely between you, your program and your preceptor. Some nursing schools require different clinical hours, some build clinicals into the coursework and some leave the format more open-ended.
How Do Clinicals Work in an Online Nurse Practitioner Program?

As an online student, you’ll choose your preceptors and select a clinical site that’s convenient for you. FNPs maintain a versatile practice, so you have plenty of options. The following settings are available for nurse practitioner clinicals:
- Family practice medical clinic
- Internal medicine outpatient clinic
- Retail clinic
- Pediatric clinic
- Women’s health clinic
- Community health center
- Urgent care clinic (non-emergency room)
Some universities will assist with site selection as well. If you encounter any problems during your search, STU can connect you with a university-partnered alternative. Florida is a big state, though, and affiliates may be up to 100 miles from your location. You should confirm your options with STU before requesting an assignment.
What’s the Process for Preceptor Selection?

Finding a clinical preceptor is crucial to your success as an FNP-in-training. Rotations expand your knowledge and skill set, so you’ll work outside your unit with a preceptor who isn’t your direct supervisor. Many MSN – FNP programs also require you to work under the supervision of nurse practitioners with at least two years of experience.
That’s the case at St. Thomas University. You also have the option to work with an M.D. or D.O. in primary care for one of your rotations. The remaining criteria are as follows:
- Preceptors must hold an unencumbered license to practice in Florida.
- Nurse practitioners must be board-certified by the ANCC or AANP.
- Women’s health nurse practitioners, however, may be certified by the National Certification Corporation (NCC).
What’s Your Scope of Practice as a Family Nurse Practitioner?
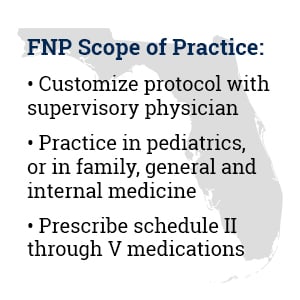
While certification and certificate programs are nationally administered, the scope of practice varies by state. In Florida, FNPs maintain a supervisory relationship with a physician. Terms are negotiated between both parties, mutually agreed upon and formalized in a written protocol. Depending on your protocol, you can prescribe medication, including controlled substances (schedule II through V). Ultimately, you’re authorized to practice in:
- Family medicine
- General medicine
- Internal medicine
- Pediatrics
You can find additional details through the AANP and the Scope of Practice Policy project. Both sites maintain a state-by-state breakdown, but if you decide to work in a U.S. Veterans Health Administration facility, you won’t need to review state guidelines. That’s because nurse practitioners in the VA have full practice authority. They can operate without a supervising physician to evaluate patients, order and interpret diagnostic tests, create and manage treatment, and prescribe medications.
How Are Nurse Practitioners Different From Physician Assistants?
Both physician assistants (PAs) and nurse practitioners are master’s-prepared, board-certified healthcare professionals who fill the gap in primary care. According to BLS, their job growth and salary are similar as well.
The American Academy of Physician Associates notes that PAs complete rigorous clinical training as part of their graduate programs, typically involving around 2,000 hours of supervised clinical rotations across medical and surgical specialties. This is often more than what is required in most nurse practitioner (NP) programs.
Additionally, PAs must complete 100 hours of continuing medical education (CME) every two years and pass a recertification exam every 10 years to maintain national certification. In comparison, nurse practitioners recertify every five years, either by exam or by meeting practice and continuing education-hour requirements.
While PAs and NPs both deliver high-quality care, their educational pathways and practice models differ. PAs earn a master’s degree through medical-model PA programs, focusing on diagnosing and managing diseases across a range of patient populations. In contrast, NPs are registered nurses who earn master’s or doctoral degrees in nursing, building on a patient-centered, holistic approach that emphasizes health promotion, disease prevention and education.
How Much Does an FNP Make?
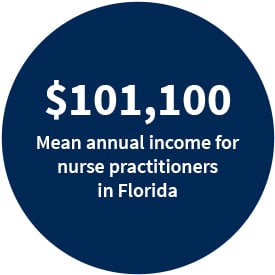
FNP salaries reflect their depth of expertise, and most nurse practitioners make between $108,000 and $150,000 a year. The salary information below is current as of July 2025.
ZipRecruiter reports earnings by state and metropolitan area. Nurse practitioners in Florida enjoy a mean annual income of $97,368. Nationally, median wages are $130,295, but Florida has a relatively low cost of living and no state income tax. As NerdWallet‘s cost of living calculator reveals, a salary of $97,368 in Los Angeles is equivalent to a salary of $76,215 in Miami. Luckily, nurse practitioners in Miami, Fort Lauderdale and West Palm Beach earn around $124,000.
Check out the list below for a sampling of nurse practitioner incomes throughout Florida, all calculated by ZipRecruiter:
- Tampa: $123,131
- Petersburg: $123,205
- Orlando: $121,547
- Sarasota: $125,569
- Big Pine Key: $138,896
- Bradenton: $118,099
- Sebring: $105,597
- Panama City: $116,262
- Port St. Lucie: $130,291
- Melbourne: $120,773
Where Do FNPs Work?

If you’re interested in where family nurse practitioners (FNPs) find the most opportunities across Florida, recent data shows that a diverse mix of organizations is actively hiring for these advanced practice roles. Health systems, retail clinics, primary care groups, hospitals and large employers each play a significant part in the state’s vibrant market for FNP talent.
Below is a list of prominent employers and networks seeking FNPs in Florida. It reflects trends from 2024 to 2025, according to job boards such as Indeed and Vivian Health, and regional healthcare employment reports from the Florida Hospital Association:
- CVS Health / MinuteClinic
- Walgreens
- Matrix Medical Network
- Lee Health
- Mayo Clinic
- AdventHealth
- Kaiser Permanente
- Planned Parenthood
- Primary Care Partners
- Baptist Health South Florida
- S. Department of Veterans Affairs (VA)
- Orlando Health
- Tampa General Hospital
- HCA Healthcare
- Florida Hospital Association members
- Community health centers and urgent care networks statewide
Are Family Nurse Practitioners in Demand?
Family nurse practitioners are in high demand. Job growth for nurse practitioners is over five times the national average. BLS also predicts that over 141,200 new NP jobs will be created between 2023 and 2033. That number doesn’t include the existing positions vacated by retiring nurse practitioners. As demand for nurse practitioners in primary care continues to rise, family nurse practitioners can anticipate a broad range of employment opportunities. In fact, nearly 90% of new NPs are trained to deliver primary care.
More patients are turning to FNPs for care, and there are over 1 billion patient visits to nurse practitioners each year. Retail clinics make a significant contribution to this trend. Also, there are just over 1,700 retail clinics operating in America. That’s because retail clinics employ nurse practitioners to increase access to primary care, and they’re doing so in the wake of a growing physician shortage. In fact, where most retail clinics accept walk-ins and same-day appointments, patients in traditional care settings often wait weeks for an appointment with their family physician.
Of new nurse practitioners are trained in primary care
– American Association of Nurse Practitioners
What’s the Career Outlook for FNPs in Florida?
Employment projections for FNPs in Florida are significantly high. BLS lists Florida in the top five states for nurse practitioner employment.
Many FNPs go on to pursue a Doctor of Nursing Practice (DNP) to further enhance their leadership, clinical and policy-making skills. You can start your journey alongside a growing number of primary care providers with an MSN – FNP online from STU.
Spotlight on the Primary Care Shortage: FNPs Fill the Gap

Predictions about the shortage of primary care providers in Florida are more urgent than ever. Recent statewide forecasts project that Florida will face a shortfall of nearly 18,000 primary care physicians by 2035.
This trend is driven by rapid population growth and the fact that almost one-third of Florida’s physicians are now aged 60 or older, with a significant wave nearing retirement. Health workforce reports indicate that many rural and underserved regions are already struggling to replace departing doctors fast enough to match patient needs.
On a national scale, the situation is equally critical. The Association of American Medical Colleges (AAMC) now predicts a nationwide shortage of up to 86,000 physicians by 2036, including major gaps in both primary and specialty care. Meanwhile, federal data show that medical school graduates choosing primary care residencies remain limited, with demand for services outpacing supply as U.S. demographics shift older and sicker. FNPs are meeting these needs in a number of ways:
- Nurse practitioners are bridging this gap, stepping in where physician numbers lag. The number of nurse practitioners practicing in the U.S. has soared to over 385,000 in 2025, with more than two-thirds providing primary care services.
- In Florida and nationwide, NPs are increasingly delivering front-line care. Over one billion patient visits are made to nurse practitioners each year, a figure that continues to rise as NPs expand their presence in family practice, urgent care, retail health clinics and rural settings.
- Non-physicians are filling the primary care gap. Non-physician clinicians, primarily nurse practitioners and physician assistants, now deliver more than a quarter of all health visits in the U.S., up from just 14% a decade ago, as patients increasingly rely on these providers for essential care.
Additionally, graduate counts reflect the field’s rapid growth. Each year, family nurse practitioner (FNP) programs graduate tens of thousands of new providers, eclipsing the number of new primary care physicians and fueling the NP workforce pipeline.
Family nurse practitioners are already stepping into expanded roles as primary care access challenges intensify across Florida and beyond. As the physician shortfall grows and retirement accelerates among existing doctors, FNPs are fundamental in ensuring patients receive timely, high-quality care in every type of community.
Are Online Nursing Students Eligible for Financial Aid?

Federal financial aid, scholarships and tuition reimbursement are all available to students enrolled in an accredited online program. You can fill out the Free Application for Federal Student Aid (FAFSA). You can also research nursing scholarships online.
Tuition reimbursement is offered by many healthcare employers as part of the benefits package. Reimbursements can reach up to $5,000 per year, but you may be required to remain with the company for a few years. If you’re a new hire, you might need to work for a set period of time before becoming eligible. Since policies and financial support vary, be sure to confirm the details with your HR department or benefits administrator.
What Is a Health Professional Shortage Designation Area and How Does It Affect Your Financial Aid?

Health Professional Shortage Areas (HPSAs) identify provider shortages in primary care, dentistry and mental health. Designations may refer to a geographic area or patient population. They may also refer to specific healthcare settings, such as state mental hospitals or correctional facilities.
Healthcare professionals who serve in Health Professional Shortage Areas (HPSAs) continue to qualify for substantial loan forgiveness and financial incentives. In 2024, the National Health Service Corps (NHSC) supported nearly 20,000 primary care, dental and mental health clinicians in HPSAs, offering up to $50,000 in student loan repayment for a two-year service commitment.
Nurses and nurse practitioners working at critical shortage facilities can also benefit from the Nurse Corps Loan Repayment Program, which covers up to 85% of unpaid nursing education debt over three years of service. Providers in HPSAs may additionally receive a 10% Medicare bonus payment for designated services, further boosting support for clinicians in underserved communities.
The U.S. Department of Health & Human Services and the Health Resources and Services Administration (HRSA) continue to prioritize funding for the following loan repayment and forgiveness programs. These initiatives help recruit and retain professionals in high-need areas such as:
Spotlight on HPSAs: The Rural Healthcare Crisis
Rural communities face a severe primary care shortage. Only 9% of U.S. physicians practice in rural areas, but over a third of Florida’s population lives in federally designated Health Professional Shortage Areas (HPSAs). By 2025, Florida had 304 designated primary care HPSAs, highlighting the depth of the access challenge.
Nurse practitioners (NPs) have become vital to bridging this gap. The percentage of rural NPs has grown by over 40% in the last decade. To attract and retain NPs in these high-need areas, several significant incentives are available:
- Florida‘s Nursing Student Loan Forgiveness Program: This program offers up to $16,000 over four years for nurses, including NPs, who work in HPSAs and other designated shortage facilities.
- NHSC Rural Community Loan Repayment Program: Provides NPs up to $105,000 in loan repayment for a three-year service commitment in rural HPSAs.
- Medicare HPSA Bonus: All eligible providers practicing in HPSAs can receive a 10% bonus on covered Medicare services, supporting the financial viability of rural practice.
These initiatives, combined with the shifting primary care workforce, are ensuring that more rural Americans have access to vital healthcare services delivered by advanced practice nurses.
Can You Use Your Military Benefits for an Online MSN FNP Degree?

Military education benefits apply to accredited schools and programs, no matter the format. That’s the case if you’re active duty, a veteran, military spouse or dependent. In fact, the VA maintains a helpful GI Bill Comparison Tool to help you estimate your funding.
St. Thomas University welcomes active-duty military members, veterans and their families. If you’d like to access your benefits for the online MSN – FNP, you can get started by calling an enrollment specialist at 855-215-4021.
How Long Does It Take to Graduate From an MSN FNP Program?
Students in a traditional, on-campus program typically complete their MSN – FNP in two to three years. Students in an accelerated online program can take less time to earn their degree. That’s because traditional courses run for 15 weeks. Accelerated courses are only six or seven weeks, so you cover the same material in half the time.
Students taking a full course load can complete the accelerated online MSN – FNP at STU in as few as 18 months. This timeline depends on your course schedule and clinical rotations. Ultimately, it’s best to work at a pace that’s sustainable for you.
How Much Time Will You Need for Your Courses?

MSN – FNP programs are academically rigorous, and accelerated online courses cover material at a swift pace. That said, you should plan to spend 12 to 15 hours a week on each three-credit course. This includes your “in-class” time, viewing video lectures, completing course modules and participating in discussion forums.
The accelerated format does require a few extra hours of study when compared to traditional courses. However, you won’t have to commute to campus or rearrange your schedule, so you’re still saving time — and speeding your path to graduation.
Can You Really Keep Your Job and Earn Your MSN Degree?
Online degrees allow you to work around your schedule. You can manage your courses, clinical hours, work commitments and personal life however you see fit. With 24/7 access, night owls and early birds are equally successful. Some study for a few hours every day, while others catch up on the weekend.
Some FNP students work three 12-hour shifts and spend the rest of the week on school work or clinicals. With dedication, you’ll be able to achieve your goal of becoming a family nurse practitioner. Stay organized by merging your calendars, planning ahead and studying at the pace that works best for you.
Will Employers Care If You Earned Your MSN FNP Degree Online?

Most healthcare employers treat accredited online MSN – FNP degrees the same as traditional on-campus programs. They focus on factors like accreditation and certification rather than the mode of delivery. In fact, the healthcare industry is ahead of the curve.
Hiring managers regularly employ online grads, but only if they attended an accredited program at a reputable institution. Over 25% of students earn their degrees entirely online. As online education continues to expand, employers have adjusted, prioritizing accredited programs and real-world clinical experience over how students earned their degrees.
In other words, an accredited online education, combined with in-person clinical rotations, provides you with the same qualifications as traditional MSN – FNP students. Note also that your STU diploma doesn’t say whether you completed your degree program online or on campus.
How Are Nursing Courses Taught Online?

Simply log in and enter your virtual classroom. From there, you can open or download the syllabus. Once you’re familiar with the course outline and important deadlines, follow clearly labelled links to access reading materials and discussion forums, view video lectures, or upload assignments.
More often than not, lessons and course modules are arranged in chronological order, so it’s easy to progress through the material. Basically, your online classroom is a bit like your online banking account. It’s tailored to you, with links for everything you need, and tech support is available if you run into any issues.
What Kind of Tech Do You Need for Online Courses?
Use your phone or tablet if you want to log in when you’re on the go. Otherwise, a computer and internet access are all you need. It’s a good idea to update your operating system and web browser before your first class. You’ll also want to confirm that your computer can:
- Play videos
- Upload and download files
- View PDFs
- Run presentation software
- Run word processing software
- Open and edit spreadsheets
Do Online Nursing Professors Have Clinical Experience?
Absolutely. Nursing programs are accredited by either the CCNE or the ACEN. Both require nursing faculty to maintain relevant clinical experience. Professors must keep their skills current by remaining in clinical practice or completing continuing education, and their knowledge must be relevant to the courses they teach.
How Will You Communicate With the Faculty?
Online faculty are available through your virtual classroom, phone and email. Some professors use video chat or text. While they aren’t available 24/7, nursing faculty keep an open dialogue with their students. Most respond within 24 hours. After all, your professors are MSN-prepared nurses (at a minimum), so they know what you’re going through.
Online students are welcome to video chat with professors during office hours (often through Zoom video conferencing). You can email or call anytime.
It is imperative that students dedicate the time to meet all their requirements. It is important to be engaged in the class and participate in discussions. It is essential to keep good communication with your instructor to facilitate your needs.
– Cassandre Milien, Clinical Coordinator, St. Thomas University Online RN to BSN Program
Which Support Services Are Available to Online Nursing Students?
Support services for online students vary from university to university. Most, however, provide tech support and digital library access. Online MSN – FNP students at STU have access to both.
Online tutoring services are available 24 hours a day. Research and writing assistance are also available. The library is your go-to for all three options, and it’s open from:
- 8:30 a.m. to 10:30 p.m. Monday through Thursday
- 9 a.m. to 4:45 p.m. on Friday
- 9 a.m. to 5 p.m. on Saturday
- 11 a.m. to 9 p.m. on Sunday
Reach out by phone or email to make a request.
Do You Have to Wait for the Fall Semester to Enroll?
Many traditional MSN – FNP programs only accept new students for the fall semester. However, St. Thomas University’s accelerated online degree offers six start dates per year.
Ready to advance your nursing career? Visit the calendar for the next enrollment period and apply today to STU’s online MSN – FNP program.