Artificial intelligence is changing the way healthcare professionals deliver patient care. Hospitals, policymakers and nurses are testing new technologies to improve clinical decisions, streamline workflows and strengthen patient outcomes. To understand the potential of AI in clinical settings, this report, conducted on behalf of St. Thomas University (STU), reviews recent findings from U.S.-based healthcare organizations, nursing foundations and policy groups.
Drawing on evidence-based research and publicly available data, this analysis explores what nurses think of AI use, where healthcare systems have adopted new tools and how states are responding with legislation. The findings offer a snapshot of the current impact of AI on healthcare, while examining its implications for nursing practice, education and public health.
Key Takeaways
- 44% of hospitals in metro counties in the U.S. reported using AI in their operations in 2025.
- 64% of nurses said they would like to see more AI tools used in their clinical work.
- Machine learning models have helped reduce mistriage rates for critically ill patients from 1.2% with traditional methods to just 0.9% with AI-powered triage.
- AI integration could free up roughly 20% of nursing time per shift, improving workflow efficiency and patient care.
- As of June 2025, 17 states have passed 27 healthcare-related AI laws, reflecting growing legislative attention, but most states are still in early stages.
Artificial Intelligence Advancements in Healthcare
Hospitals are increasingly adopting artificial intelligence to support clinical practice. These AI technologies aim to improve clinical decision-making, streamline patient care and enhance patient safety by reducing errors. From predictive analytics in triage to AI-driven patient monitoring, the use of AI reflects a shift toward regular applications of artificial intelligence in hospital operations.
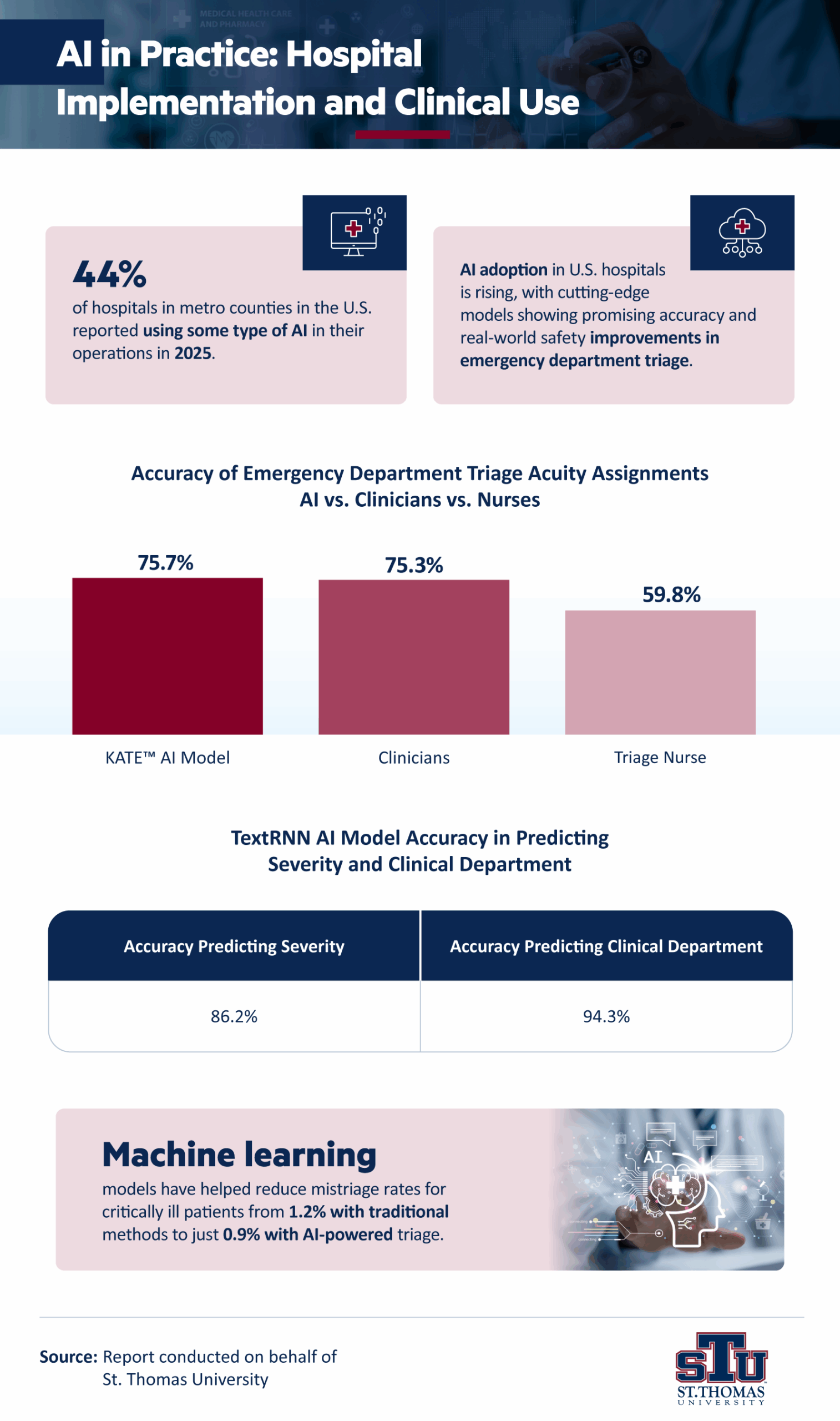
In 2025, nearly 44% of hospitals in metro counties across the U.S. reported using artificial intelligence in their operations. This adoption highlights the growing role of AI systems in healthcare settings where algorithms are helping clinicians make real-time decisions supported by automation and high-quality patient data.
Emergency departments provide one of the clearest examples of how AI-powered tools improve outcomes. Machine learning models have helped reduce mistriage rates for critically ill patients from 1.2% under traditional methods to 0.9% with AI-powered triage, according to a Cureus article on AI use in emergency department triage. Mistriage occurs when patients are incorrectly assigned an acuity level, either as undertriage, which delays treatment, or overtriage, which strains resources. By improving accuracy in acuity assignment, AI-based systems directly impact patient safety and ensure timely interventions for the most urgent cases.
The Emergency Severity Index (ESI) guides how clinicians assign patient acuity. It is a five-level scale used nationwide, where Level 1 requires immediate life-saving intervention, and Level 5 is the least urgent. Studies have shown that the KATE™ AI model achieved 75.7% accuracy in ESI assessments, nearly matching clinicians at 75.3% and significantly outperforming triage nurses at 59.8%, according to the Cureus article.
Another algorithm, TextRNN, demonstrated over 86.2% accuracy in predicting patient severity and 94.3% accuracy in assigning the correct clinical department. These findings show how AI algorithms can enhance clinical decision-making by supporting critical thinking and improving patient outcomes.
How Nurses Feel About AI in Nursing Practice Workflows
Nurses are at the center of patient care, and their perspective is vital for understanding the integration of AI tools in clinical practice. Research shows that nursing professionals recognize AI’s potential to streamline workflows and improve patient outcomes, yet they also highlight concerns about its impact on patient interactions and the role of nurses in shaping how new technologies are implemented.
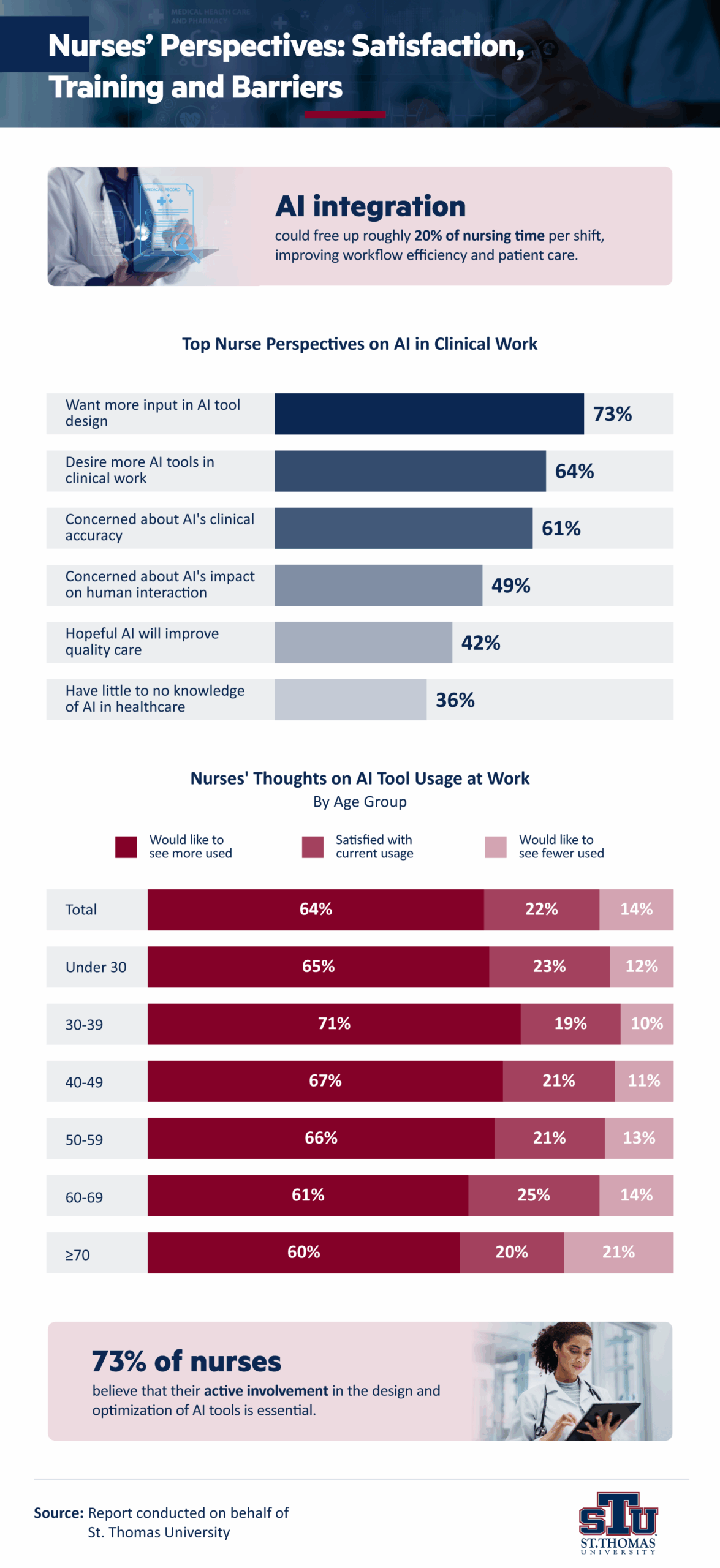
A nationwide survey of 7,200 nurses by the American Nurses Foundation (ANF) provides insight into nurses’ views on AI in healthcare. Sixty-four percent of respondents said they would like to see more AI tools used in their clinical work. The ANF and McKinsey also estimated that AI could free up roughly 20% of nurses’ time per shift by reducing administrative tasks and routine documentation.
At the same time, nurses identified areas of concern. Nearly half (49%) worried about AI’s effect on human interactions, especially the nurse-patient relationship. Another 61% were not sure if they could trust AI tools’ clinical accuracy and saw this as a top barrier to adoption. And although 42% expressed hope that AI could improve the quality of care, others emphasized the need for transparency in clinical decision support systems and stronger safeguards to protect patient safety.
Education also emerged as a pressing issue, as 36% of nurses reported limited or no knowledge of how AI is currently used in healthcare settings. This finding underscores the importance of nursing education, informatics training and leadership in preparing nurse practitioners, nurse leaders and nursing assistants to work with AI technologies.
McKinsey also noted that nurses want a stronger voice in AI integration. Nearly 3 in 4 (71%) said they want more involvement in AI tool design, implementation and optimization to ensure that interventions align with real clinical needs. Many also desired clear evidence of AI’s effectiveness and safety (69%), plus stronger guidelines and regulatory oversight. AI’s impact on nursing practices could depend on how well healthcare workers are included in decision-making and how closely new tools align with evidence-based care.
Overall, nurses are cautiously optimistic about AI’s potential. They see opportunities to streamline workflow, reduce staffing pressures and support real-time interventions, but they also insist that integration of AI must reinforce and not replace the values of high-quality nursing care.
How States Are Regulating AI in Healthcare
AI adoption in healthcare delivery is advancing more quickly than the laws that govern it. Policymakers across the country are creating new initiatives to guide how AI systems can be applied in clinical and administrative settings. These efforts reflect both the promise of AI-assisted tools and the ethical considerations of using them in direct care, insurance processes and patient interactions.
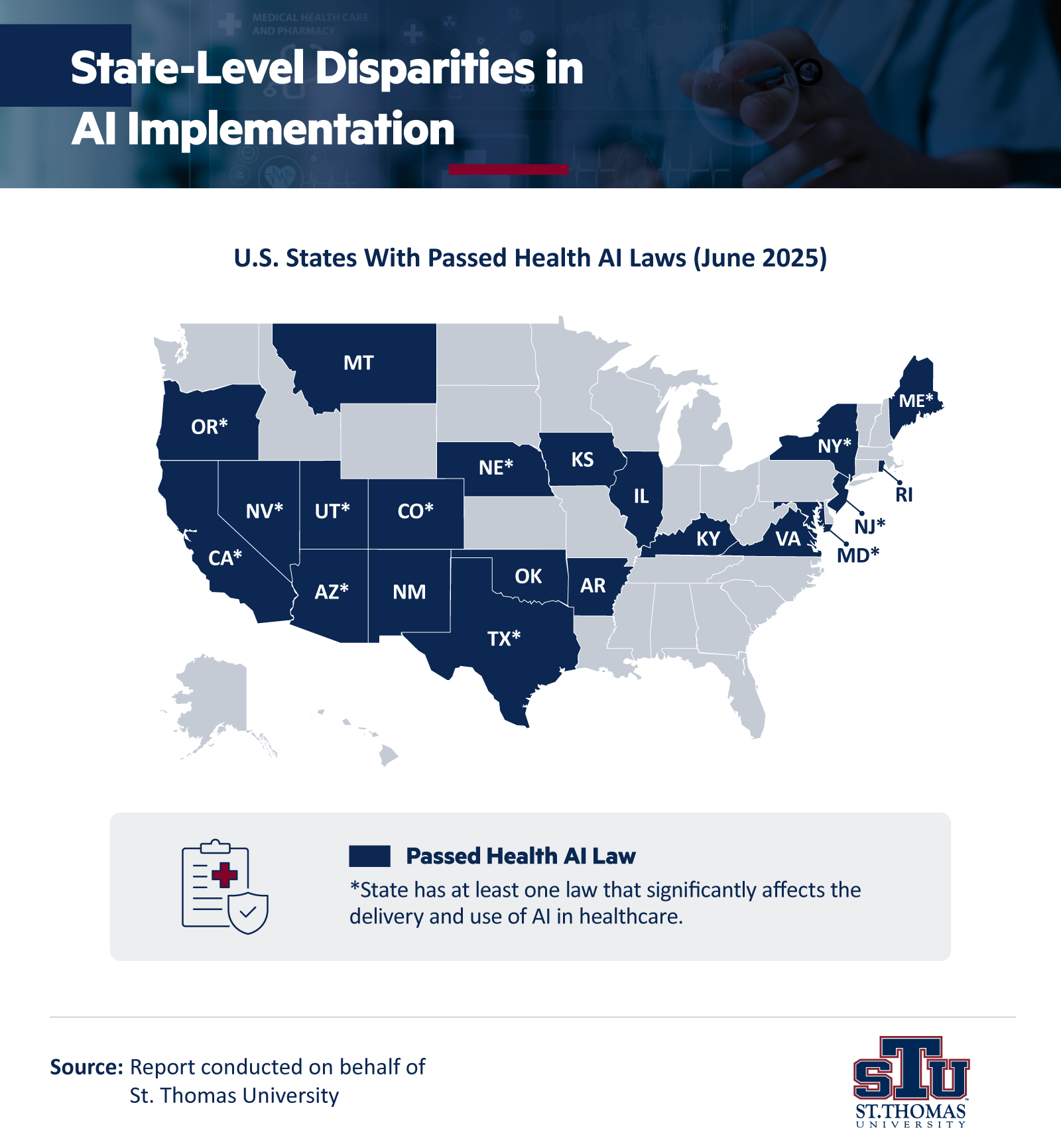
As of June 2025, 21 states have laws about AI use, but only 17 have passed significant healthcare-related AI laws. Most remain in the early stages of adoption. California, Colorado, Massachusetts, Michigan, Ohio, Pennsylvania and Wisconsin are leading with policies focused on transparency, consumer protections and provider oversight. Yet, others have yet to move beyond exploratory stages, creating disparities in how patients experience AI-driven healthcare across the country.
Some laws also address specific applications. For example, Utah, New York, Nevada and Texas regulate the use of AI-enabled chatbots in mental healthcare to prevent misrepresentation and improve crisis detection, while Arizona, Maryland, Nebraska and Texas require physician review of AI-generated insurance denials.
Other states have enacted rules designed to safeguard patients during clinical delivery. Nevada, Oregon and Texas now require disclosure when AI is used in care and prohibit AI systems from presenting themselves as human providers. These guardrails reflect the need to balance technological advancements with patient trust, while acknowledging that healthcare settings must remain transparent about how AI technologies are applied.
State policies have also been focusing on preventing algorithmic bias, ensuring clinical accuracy and strengthening patient rights to contest AI-driven decisions. These measures emphasize caution while still allowing healthcare workers and providers to test applications ranging from natural language processing to wearable monitoring devices and robotics. These emerging policies illustrate how state-level regulation is beginning to define the boundaries for artificial intelligence in nursing and other areas of healthcare delivery.
AI in Practice
Artificial intelligence is already influencing how hospitals deliver direct patient care, how nurses manage their workflows and how states regulate clinical innovations. The research shows both the promise and the challenges of AI integration, from improved triage accuracy to concerns about patient interactions and ethical safeguards.
As adoption expands, the role of nurses, educators and policymakers will be essential in guiding the use of AI technologies across healthcare settings. With careful attention to evidence-based practice, ethical considerations and patient outcomes, AI has the potential to support the critical thinking and compassion at the heart of nursing care.
For nursing students, these developments underscore the value of building strong foundations in nursing education and leadership. Gaining familiarity with AI tools and their applications in healthcare delivery can prepare future nurses to influence how technology is used while ensuring patient care remains centered on human connection.
Methodology
Conducted on behalf of STU, this report draws exclusively on recent research from U.S.-based nursing, healthcare and policy organizations to explore how artificial intelligence (AI) is reshaping nursing practice and patient care. This report includes analysis of publicly available data, national reports and peer-reviewed studies published by leading institutions, including:
- American Nurses Foundation (2024)
- McKinsey & Company (2024)
- National Institutes of Health (NIH)
- Louis Federal Reserve (2025)
- American Medical Association (AMA)
- Manatt Health (July 2025)
- Chief Healthcare Executive (June 2025 article)
About St. Thomas University
St. Thomas University prepares students for leadership across the nursing profession by combining academic rigor with compassion and service. Its flexible online Master of Science in Nursing (MSN) programs allow students to advance their nursing education while balancing work and family commitments. The curriculum emphasizes evidence-based nursing practice, patient care excellence and the critical thinking skills needed to become effective nurse leaders and nurse practitioners in today’s healthcare environment.
Fair Use Statement
This article includes insights and findings from publicly available sources for educational and informational purposes. All references are credited to their original authors and organizations. Content is used under fair use principles to support research, teaching and commentary related to healthcare, nursing practice and the application of AI in clinical settings.